
- support
- info@evidentic.com
- +49 (0) 30 959 99 8831
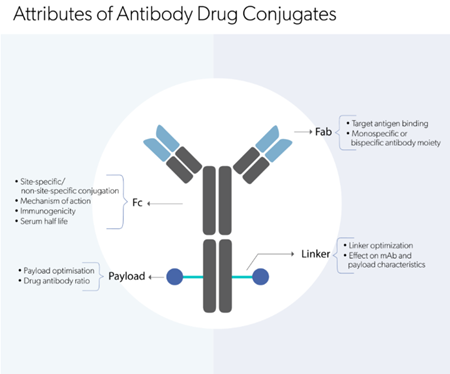
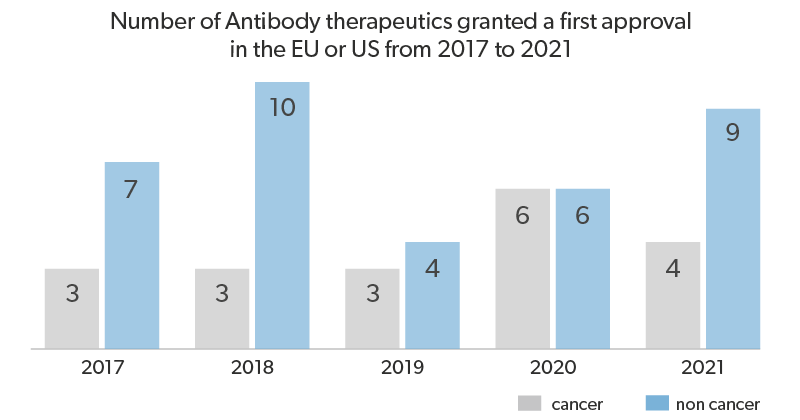
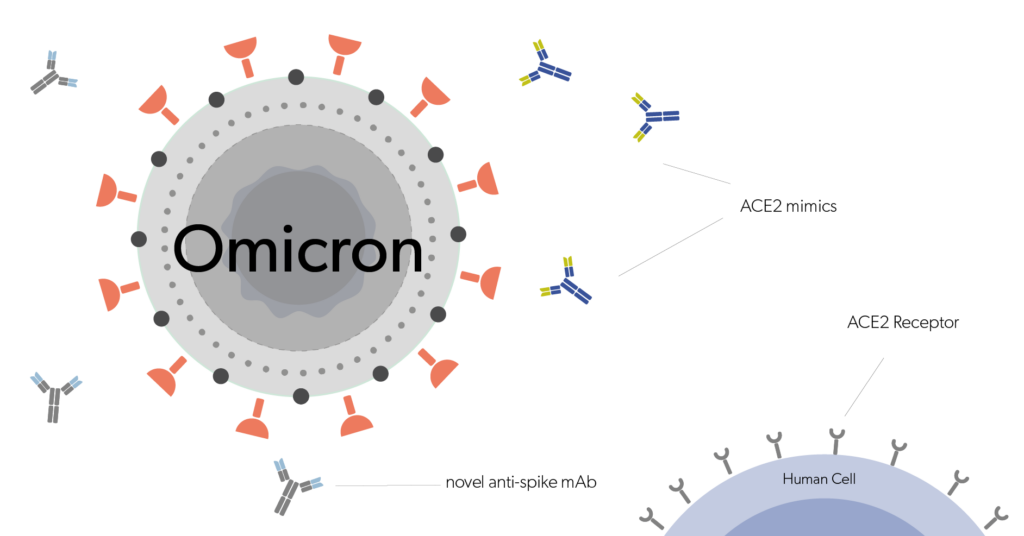
Biologic products have revolutionized the pharmaceutical industry. But these drugs, including the monoclonal antibodies (mAbs), when administrated into patients may provoke an immune response leading to the development of anti-drug antibodies (ADAs). With a boom in the biologics market and the rise of novel antibody formats, such as bispecifics, antibody fragments, and antibody conjugates, immunogenicity evaluation has become an important criterion.
Factors that determine the immunogenicity of a biologic drug can be:
Comprehension of the incidence or implications of ADA that may undesirably affect the product’s pharmacokinetic profile, pharmacodynamic effect, clinical efficacy or safety pivotal in any therapeutic protein product development program. Hence immunogenicity produced by biotherapeutics has garnered significant attention from regulatory bodies, industry and clinicians.
ADAs that develop in patients treated with a biologic drug can be categorized into two main types:
1. Neutralizing block and directly interfere with the drug’s ability to bind its target;
2. Non-neutralizing ADAs that recognize other epitopes on the drug while still allowing the antigen-binding activity. For example, antibodies against the Fc region of the drug.
Determination of neutralizing and non-neutralizing ADAs in serum samples is important for drug development’s preclinical and clinical phases. The process involves (1) Screening assays, (2) Confirmatory assays, and (3) Characterization assays.
These techniques detect the presence of ADAs in the therapeutic protein. Following the administration of biotherapeutic products, the screening assays evaluate unique polyclonal antibodies in each patient sample and between patient samples. Methods such as enzyme-linked immunosorbent assays (ELISAs), radio-immunoprecipitation assays (RIPA) and newer technologies such as electrochemiluminescence (ECL), bead-based assay, Gyrolab system, surface plasmon resonance (SPR), biolayer interferometry can be availed in the primary screening assays to determine immunogenicity.
The platforms developed for screening ADAs must consider:
All screening assays developed to detect biotherapeutic products must be optimized and validated within respective laboratories for reproducibility and accuracy. Interpretation of the screening assay results as antibody-positive or antibody-negative is defined by a ‘cut-point’ (threshold) strategy.
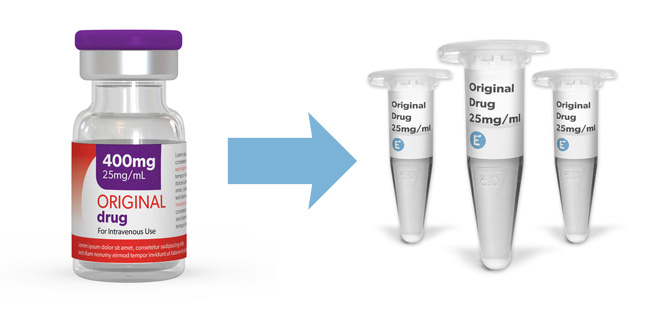
Buy approved biologic drug aliquots from Evidentic as calibrators for ADA assays.
These assays confirm the specificity of ADAs to the particular therapeutic antibody. This approach eliminates the false positive samples identified in the screening assay by the addition of excess antigen to both treated and untreated samples in the same assay. The presence of ADAs in the sample is confirmed through a signal reduction in the treated versus the untreated sample.
Once the presence of ADAs to a particular drug is confirmed, it is important to characterize the ADAs. Characterization of positive samples titre determination, evaluation of neutralization potential, elucidation of the immunoglobulin class and subclass, isotype, etc. These factors provide a better understanding of the immunogenicity of the biologic drug and its clinical impact. In this regard, neutralization assays are vital in assessing the ability of ADAs to neutralize the biological activity of the therapeutic antibody. Cell-based bioassay or a non-cell based competitive ligand binding (CLB) assay are the two main in vitro methods available for detecting neutralizing ADAs and must be utilized based on parameters such as time consumption, easy to implement protocols and appropriate detection of the impact on drug efficacy.
Anti-idiotype antibodies (anti-IDs) are ADAs that specifically bind to the antigen-binding site, within the Fv region (also known as the idiotype) of an antibody-drug. The current generation of approved antibody drugs is humanized or fully-human, in which the idiotype is the only “foreign” sequence. Hence, anti-IDs are usually the most common ADAs generated in response to the majority of antibody drugs.
Read more: The advent of therapeutic antibodies
Apart from that, anti-IDs have become important in-vitro diagnostic tools for immunogenicity and pharmacokinetic studies. For assay development, anti-IDs against a biologic drug are generated in animal models, usually mouse/rabbit mono- or poly-clonal. Depending on the binding site of the anti-ID on the Fv of the antibody drug, anti-ID antibodies can be neutralizing or non-neutralizing, and are classified into three types:

In-vitro assays employing anti-IDs, along with polyclonal ADAs, are used for immunogenicity studies. However, anti-IDs are more commonly used for pharmacokinetic (PK) studies. Since PK studies look into drug metabolism, anti-IDs particularly help detect bound or unbound drugs in the serum, urine and other body fluids.
Moreover, with regard to biosimilar development, anti-IDs are an important tool for immunogenicity comparability studies. During the early phase of biosimilar development, screening and functional assays utilizing anti-IDs can help confirm the antigenic specificity of biosimilar candidates to the originator molecule or the reference product. Some of the commonly used assays to confirm the specificity of biosimilars include:
In addition, comparative clinical trials are conducted to evaluate the immunogenicity of biosimilars and the reference product. These trials must be conducted in the most sensitive patient population and use of same clinical protocols (for example, routes of administration, treatment schedules, sampling procedures, sampling time points including baseline/pre-treatment sample and storage conditions) and antibody assays for the generation of valid comparative data. The amount of immunogenicity data required is dependent on experience gained with the reference product and/or the product class. Such evidence-based data help clinicians/physicians dismiss concerns about switching their patients to biosimilars or among multiple biosimilars.
Evidentic offers analytical quantities of commercially approved biologics and therapeutic antibodies (chimeric, humanized and fully human mAbs) that can be used as calibrators, positive, negative or quality controls for developing and manufacturing in-vitro diagnostic assays.
Evidentic aliquots are ideal for the development of anti-idiotype antibodies, anti-drug antibody (ADA) detection assays and other in vitro diagnostic assays utilizing anti-human conjugated secondary antibodies.
Wadhwa M, Knezevic I, Kang HN, Thorpe R. Immunogenicity assessment of biotherapeutic products: An overview of assays and their utility. Biologicals. 2015;43(5):298-306. doi:10.1016/j.biologicals.2015.06.004
Großerichter-Wagener C, Kos D, van Leeuwen A, et al. Biased anti-idiotype response in rabbits leads to high-affinity monoclonal antibodies to biologics. MAbs. 2020;12(1):1814661. doi:10.1080/19420862.2020.1814661
Harth S, Frisch C. Recombinant Anti-idiotypic Antibodies in Ligand Binding Assays for Antibody Drug Development. Methods Mol Biol. 2021;2261:291-306. doi:10.1007/978-1-0716-1186-9_18
Schreitmüller T, Barton B, Zharkov A, Bakalos G. Comparative immunogenicity assessment of biosimilars. Future Oncol. 2019;15(3):319-329. doi:10.2217/fon-2018-0553

Evidentic GmbH
Martin-Buber-Str. 10
14163 Berlin