
- support
- info@evidentic.com
- +49 (0) 30 959 99 8831
Cell therapies are an innovative and promising class of biologic drugs against cancer. Genetically engineered immune cells have emerged as a powerful treatment modality to redirect immune cells to target and eliminate cancer cells. This type of cellular immunotherapy, often known as adoptive cell therapy, is achieved by deploying Chimeric Antigen Receptors (CARs) to a specific antigen, on the surface of immune cells. The success of CAR T-cells against B-cell malignancies has indeed revolutionized the treatment strategies for haematological cancers. However, the toxicities associated with CAR-T cells and their limited success against solid tumors have led to several generations of CAR constructs and the exploration of other CAR-engineered immune cells, including CAR-NK cells, CAR-NKT cells, CAR-macrophages and CAR-γδ T cells.
CAR cell therapy utilizing T-cells to override the deception developed by the cancer cells are known as CAR T-cell therapy. In this treatment modality, the patient’s T-cells are collected and genetically modified to express the chimeric antigen receptors on their surface. This allows the genetically engineered T-cells to target and selectively kill cells expressing the specific antigen actively. They are then expanded in the laboratory and re-infused into the patient. Advantages of CAR T-cell therapy are
Furthermore, CAR-T-cell therapy is a single short treatment with mostly two weeks of inpatient care.
Presently, CAR-Tcell therapy, with 500 CAR-T cell trials being conducted worldwide, has been adopted to treat various cancers. The efficacy of various clinical trials of CAR-T cell therapies can vary with the use of different sources, preparation techniques of CARs and T cells, along with differences in pre-treatment and combinations of drugs. However, reports suggest CAR-T cells be effective in treating tumors with an efficacy rate of 30% to 70% or even more than 90%. The four CAR-T cell products currently available on the market are Kymriah®, Yescarta®, Tecartus™ and Breyanzi®.
A CAR comprises several domains, the 3 most important being
This extracellular domain helps to identify the target antigen and redirect the specificity of CAR-expressing lymphocytes. This portion of the CAR consists of a single-chain variable fragment (scFV) obtained from a monoclonal antibody(mAb) such as the mouse anti-human CD19 antibodies (for example, Breyanzi, Yescarta®), and is the crucial factor in determining an effective CAR function.
The hinge of CARs links the extracellular antigen-binding domain to the intracellular signalling domains. Hinges render flexibility and appropriate length to access the target antigen. CAR hinge domains contain amino acid sequences from CD8, CD28, IgG1 or IgG4. The features of the hinge determine cytokine production and activation-induced cell death (AICD) of CAR T cells.
The transmembrane portion offers stability by anchoring CAR in the T cell membrane and facilitates CAR function. Usually comprises type 1 proteins such as CD3ζ, CD28, CD4 or CD8α, depending on which the intensity of stability, dimerization and incorporation into endogenous TCRs may vary.
A T cell activation domain is derived from the CD3ζ chain of the T cell receptor and the co-stimulatory domains that contain the immunoreceptor tyrosine-based activation motif-containing regions of CD28 or 4-1BB (also known as CD137 and TNFRSF9) form the intracellular signalling domain.
Also, engineered CAR T cells functions can be further enhanced with the presence of a cell surface or secreted immunomodulatory molecule. Modified CAR T cells with new designs are focused on improving the safety and efficacy of CAR-T cell therapy.

Natural Killer (NK) cells are cytotoxic cells, functionally similar to T-cells but lack the antigen-specific TCR. The intrinsic ability of NK cells to recognize the absence of HLA-proteins makes them potent killers of tumor cells and virus-infected cells. Hence, engineered CAR-NK cells targeting tumor-specific antigens can offer a powerful cytotoxic capacity combined with specificity. Moreover, the absence of TCR-mediated killing makes them ideal candidates for allogeneic cell therapy, circumventing the risks of graft vs host disease (GvHD).
Pre-clinical studies and clinical testing of CAR-NK cells for cancer immunotherapy have shown promising results, with several advantages over CAR-T cell therapy such as:
To date, most of the CAR-NK cell research has utilized CAR constructs designed for CAR-T cell therapies. However, new-generation CARs for NK cells are under development. The proposal of “off-the-shelf” cell immunotherapy products using CAR-engineered NK cells have sparked a growing interest in this area. NK cells can be derived from multiple sources, including NK92 cell lines, peripheral blood mononuclear cells (PBMCs), umbilical cord blood (UCB), and induced pluripotent stem cells (iPSCs), thus considerably saving time and cost compared to autologous CAR-T cells.
Macrophages are potent cancer eliminating cells that have phagocytic and antigen-presenting properties. They are the most abundant immune cells found within the solid tumor micro-environment and have a comparatively greater infiltrating capacity. These features have led to the conception of CAR-M cells. Engineered CAR-M cells are being developed as a personalized autologous treatment to induce a more targeted phagocytic activity against tumor cells. Although still in its infancy, pre-clinical evaluation of anti-HER2 CAR-M therapy has been quite encouraging. CAR-Ms have shown >75% efficacy in in-vitro and in-vivo models. Moreover, CAR-Ms have also demonstrated resistance to immunosuppressive microenvironments.
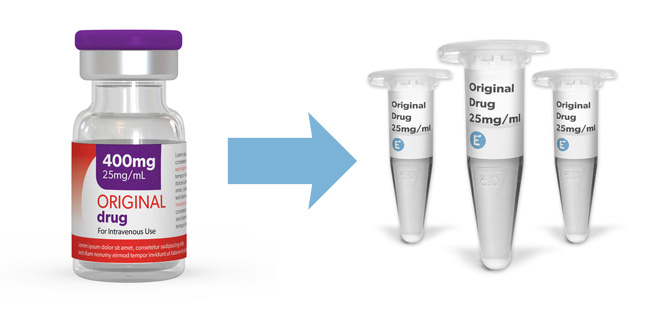
Evidentic provides analytical quantities of clinically approved biologic drugs for research use. Buy clinically EU-approved biologics in aliquot format of therapeutic clinical-grade molecules for your early drug development programs, including early phase CAR development and lead optimization.
Discover clinical-grade molecules for your research

Evidentic GmbH
Martin-Buber-Str. 10
14163 Berlin