
- support
- info@evidentic.com
- +49 (0) 30 959 99 8831

By loading the video, you agree to YouTube’s privacy policy.
Learn more
Introduction
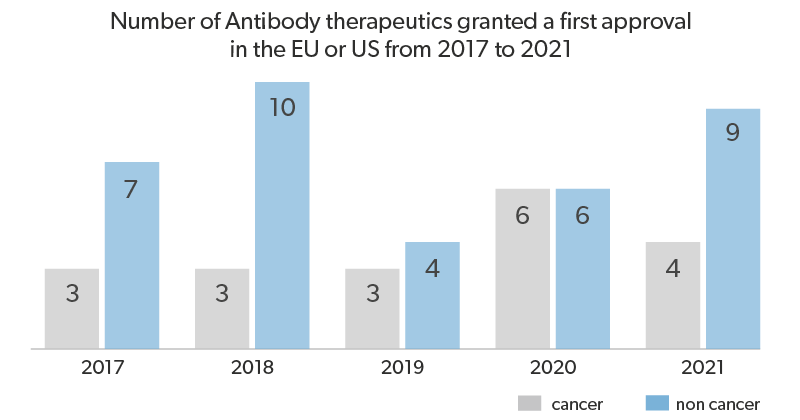
Monoclonal antibodies targeting inhibitory receptors on the surface of T-cells and cancer cells, widely known as checkpoint inhibitors, have brought antibody therapies to the forefront of cancer immunotherapies. In 2017, pembrolizumab, an antibody therapy which acts as a checkpoint inhibitor blocking the inhibitory receptor PD-1, became the first therapy that was FDA-approved for cancers with specific molecular characteristics, namely PD-1 expression, regardless of site in the body. Pembrolizumab and other checkpoint inhibitors were available to 43% of cancer patients in 2018, following their initial approval in 2011. Over that same period, the number of clinical trials involving checkpoint inhibitors grew from 215 to over 1500.7 Building on the success of checkpoint inhibitors, the future of antibody-based cancer therapies looks to an innovative new approach: bispecific antibodies (bsAb). BsAbs work by binding two different target surface markers, engaging immune cells in close proximity with cancer cells. This essay will review the mechanism of action of bispecific antibodies and new approaches to expand the therapeutic efficacy of bsAbs.
Mechanism of Action and Current Therapeutics
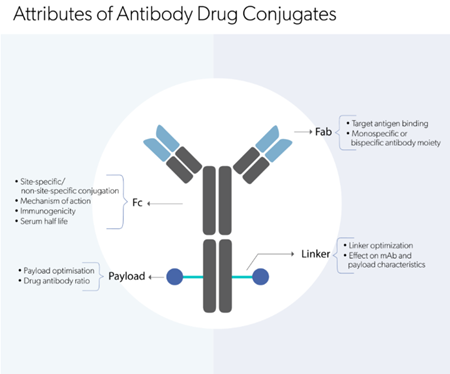
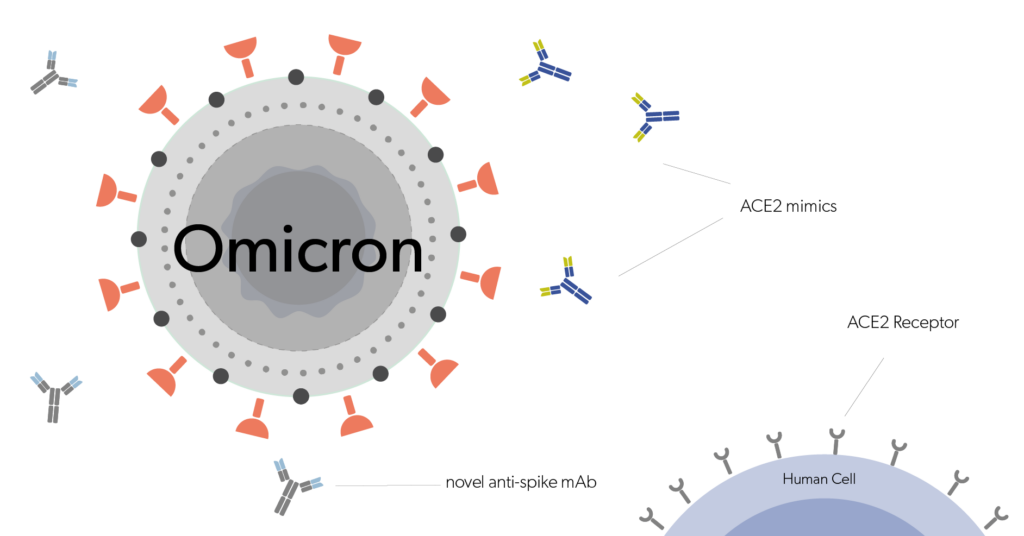
Antibodies are proteins produced by B lymphocytes in the immune system which can specifically bind to a particular antigen target. While the antigen binding sites of the antibody bind the target, the Fc portion of the antibody can bind various cells of the immune system, inducing opsonization, engulfment of the target cell by immune cells, and antibody-dependent cell cytotoxicity, killing of the antibody-bound target cell by immune cells. BsAb’s ability to engage two different target antigens simultaneously allows for the immune system to be engaged through different mechanisms. Primarily, bispecific antibodies which bind a T-cell associated antigen and a tumor antigen can engage tumor cells and T cells in close proximity, while the Fc portion of the antibody engages Fc receptors to recruit natural killer cells, dendritic cells, macrophages and other immune cells to stimulate a further anti-tumor immune response (fig 1). Recruiting immune cells to the tumour site is a major challenge in cancer immunotherapy, one that can be elegantly addressed by re-engineering our body’s own immune honing mechanisms to promote localization and activation of immune cells in the tumor microenvironment.

Figure 1. The different immune mechanisms which are engaged to kill tumor cells by using bispecific antibodies as a tumor therapy.1
The first bsAb to be FDA approved for cancer therapy was blinatumomab in 2014 for the treatment of precursor B cell acute lymphoblastic leukemia (pre-B ALL).2,3 Blinatumomab works by binding to both CD19, a protein/marker expressed on all B cells, and CD3, a T-cell marker. By engaging both markers simultaneously, blinatumomab is able to localize host T cells to cancerous B cells, thereby increasing their chances of T-cell killing. Blinatumomab almost doubled the survival of patients with pre-B ALL, compared to standard chemotherapeutics.2 Hoping to replicate blinatumomab’s success, new tumor antigen targets, including CD123, CD33, CD38, and BCMA are currently being explored for other hematological malignancies, with BCMA bsAbs currently in phase II clinical trials for multiple myeloma.4,5 In addition to new targets being explored for blood-based cancers, combination therapy with biAbs and checkpoint inhibitors is being explored to allow endogenous T-cells to localize to solid tumors and become activated despite the immunosuppressive tumor microenvironment6.
Blinatumomab, and the resulting expansion of cancer antigen targets and combination therapy regimens have culminated in more than 50 bispecific antibodies currently in clinical trials for various cancer types. These range from engaging T-cells with a cancer antigen, to targeting activation of NK cells and macrophages, overall building a repertoire of bsAbs that can be deployed for a variety of cancer antigens and different immunosuppressive microenvironments.
Research and Future Directions
One of the main challenges in tumor antigen-targeting immunotherapies is antigen escape or antigen heterogeneity. Antigen heterogeneity refers to the idea that only a portion of the cells in the tumor will express the target antigen, and antigen escape refers to the process of a small subset of antigen negative cells being enriched within the population due to the selective pressure of the antigen positive tumour cells being killed. Novel bispecific antibodies address this issue by targeting antigens that are at the heart of driving cancer development: RAS and p53.
RAS and p53 are among the most commonly mutated genes across all human cancers. Around 25% of all human cancers carry a gain-of-function mutation in RAS genes, and p53 mutations are present in 5.8% to 47.8% of tumors depending on tumor type.8,9 These high-prevalence targets across various tumor types present an opportunity for a broad-spectrum therapeutic approach, though no small molecule inhibitors of these pathways have been successfully brought into the clinic. Hsiue et al. 2021 addressed this issue by creating a bsAb which binds a commonly mutated form of p53 presented on MHC.10 This antibody bound to the mutated p53 at a higher specificity than other healthy peptides, limiting any potential off-target effects, and successfully activated T-cells and induced tumor regression in mice. Both p53 and RAS have previously been challenging to target due to their low surface expression on cells. This requires the drugs which target them to be high specificity and induce a potent immune response – properties which antibodies have innately. Douglass et al. 2021 generated various single-chain antibody fragments which bound to mutated RAS protein presented on MHC and successfully generated a bsAb which recognizes mutated RAS protein and CD3. This therapeutic resulted in potent binding to mutated RAS on the surface of multiple different cancer cell types, and activation of T-cells. These two approaches lay the groundwork for future bispecific antibodies to be developed which target tumor associated antigens that are expressed at low levels on the cell surface: targets that previous small molecule drugs could not reach.
Conclusion
Antibody therapeutics have revolutionized current cancer treatments and brought cancer immunotherapies to the forefront. Bispecific antibody therapies represent a new wave of antibody-based cancer immunotherapies which harness the specificity and innate immune potential of antibodies to engage tumor-derived antigens and immune cells to produce a powerful anti-tumor immune response. Now, a new wave of novel bispecific antibodies addresses a wider range of tumor types by creating potent responses to tumor derived antigens expressed at very low levels on cell surfaces.
BIBLIOGRAPHY

Evidentic GmbH
Martin-Buber-Str. 10
14163 Berlin