
- support
- info@evidentic.com
- +49 (0) 30 959 99 8831
The emergence of immunotherapy has revolutionized the treatment of cancer. Unlike traditional non-specific approaches such as surgery, radiation, and chemotherapy, immunotherapy provides precision-based treatment using biological agents (for example, therapeutic antibodies) to enhance immune activation and eliminate cancer. Evolving and promising types of cancer immunotherapy in clinical practice are cytokine therapies, adoptive cell transfer, and immune checkpoint inhibitors (ICIs). Other immunotherapy approaches under consideration include oncolytic virus therapies, cancer vaccines, gamma-delta T-cell therapy, CAR-M (chimeric antigen receptor-Macrophage) therapy. Interestingly, clinical trials on immune checkpoint therapeutic antibodies have shown long-term benefits in 40% of melanoma patients, 80% of Hodgkin’s lymphoma patients, and 50% of Merkel cell carcinoma patients. Therefore, among all immunotherapy approaches, immune checkpoint inhibiting therapeutic antibodies have garnered the most attention.
The activation of T-cells requires two different signals, that come from
These series of co-inhibitory and co-stimulatory receptors and their ligands are known as immune checkpoints.
Antigen/MHC-TCR binding accompanied by co-stimulatory signal will result in T-cell proliferation. In contrast, co-inhibitory signals keep immune responses at bay to prevent the destruction of healthy cells in the body or an auto-immune condition. These co-signaling molecules are found on T cells, antigen-presenting cells (Macrophages, B-cells, Dendritic cells) and tumor cells. Their interactions within the tumor microenvironment result in inhibitory or stimulatory immune signaling pathways (see Figure below).

At times, cancer cells manipulate these molecules and turn off the T-cells to evade immuno surveillance. Hence, the blocking of immune checkpoints using specifically designed monoclonal antibodies (mAbs) inhibits the stop-signals and restores the anti-tumor activity of the immune system.
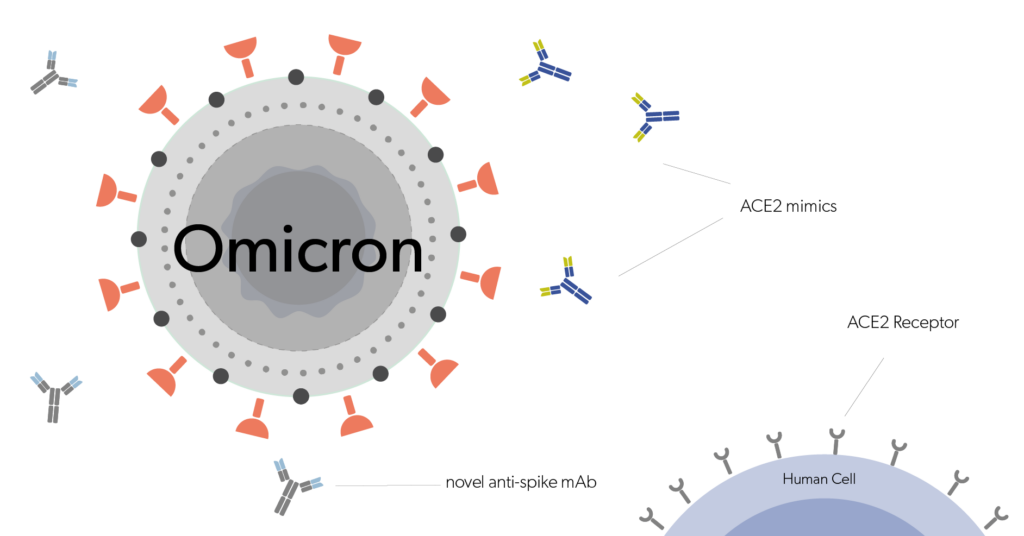
In this type of treatment, the patient receives an infusion with therapeutic antibodies, which are transported through the blood to the tumor site. The therapeutic antibodies subsequently block the receptor-ligand binding responsible for the stop–signal coming from the cancer cell and the T-cell, thereby preventing the cancer cells from restraining the T-cell activity. But, T-cells can receive different types of immune-inhibitory signals from cancer cells. For each of these stop signals, different therapeutic antibodies or ICIs are being developed. Currently, the most successful immune checkpoint inhibiting biologic drugs are therapeutic antibodies targeting the PD-1/PD-L1 and CTLA-4 pathway.
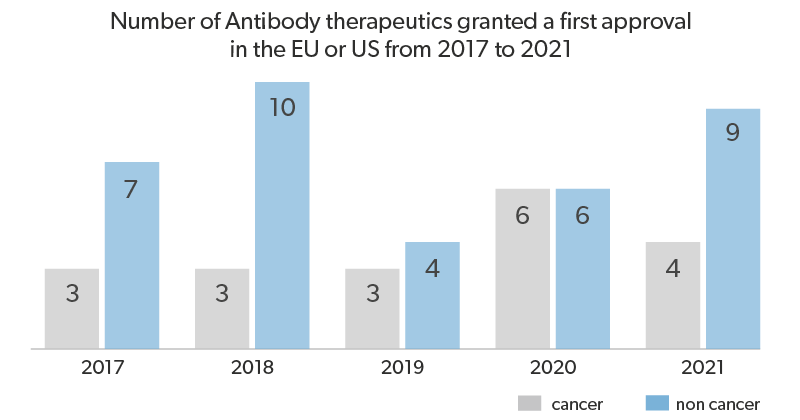
A number of monoclonal antibody drugs targeting immune checkpoint pathways have been approved for several malignancies by the US-FDA and EMA over the last few years. Although most of the currently approved therapies revive T-cell activation, NK-cell-based immune checkpoint inhibition is a promising area of research. Here we look at some of the commercially successful therapeutic antibodies as immune checkpoint inhibitors, as well as some of the emerging targets and therapeutic strategies.
Cytotoxic T-lymphocyte-associated protein 4 (CTLA-4) or CD152 is a member of the B7/CD28 proteins that inhibit T-cell activity. Regulatory T cells (Tregs) mainly express CTLA-4 but upon activation, it can be upregulated by other T cell subsets, particularly in CD4+ T cells. Immunosuppression via CTLA-4 is mediated by binding to ligands CD80 and CD86 with higher affinity, thereby blocking their binding to the co-stimulatory receptor CD28.
The first immune checkpoint inhibitor drug to be approved was the anti-CTLA-4 therapeutic antibody Ipilimumab. Another CTLA-4 therapeutic antibody under investigation is Tremelimumab (yet to be approved). In contrast, CTLA-4 mimetics can be used to suppress immune activity in auto-immune disorders. One such approved biologic drug is the fusion protein Abatacept.
Programmed cell death protein 1 (PD-1), also known as CD279, is a type I transmembrane protein receptor that is inducibly expressed after activation by TCR/antigen-loaded MHC and CD28/B7 interactions. Hence, PD-1 appears on antigen-experienced memory T-cells in peripheral tissues and less commonly on B cells, activated monocytes, dendritic cells (DCs), and natural killer (NK) cells. Activation of PD-1 signalling negatively regulates T-cell-mediated immune responses in the peripheral tissues, preventing autoimmunity and protects tissues from immune-mediated tissue damage, maintaining peripheral T-cell tolerance in normal tissues. Such crucial roles of PD-1 signalling pathways are exploited by cancer cells to evade immune surveillance and induce tumor progression. Thus, PD-1 is highly expressed in tumor-infiltrating lymphocytes (TILs) in a large proportion among many types of cancers. Therefore, therapeutic antibodies (mAbs) are designed to bind to the PD-1 receptors and play a pivotal role in preventing the escape of cancer cells.
EMA and FDA-approved ICIs against PD-1 are Pembrolizumab for melanoma, non-small cell lung cancer (NSCLC),head and neck squamous cell carcinoma, Nivolumab for melanoma, squamous cell lung cancer(SCLC), renal cell carcinoma(RCC), and Hodgkin’s lymphoma and Cemiplimab for cutaneous squamous cell carcinoma (CSCC).
PD-L1 (also known as B7-H1 or CD274) is a member of the B7 family of type I transmembrane protein receptors. The protein is predominantly expressed on many cell types such as antigen-presenting cells (APCs), T cells, B cells, monocytes, and epithelial cells. PD-L1 is the ligand for PD-1 and their interaction results in the prevention of auto-immunity and maintenance of peripheral T cell tolerance in healthy cells. Apart from binding PD-1, PD-L1 also interacts with B7 (CD80, CD86), inducing negative signals on T cells and reduces anti-tumor activity.
The EMA/FDA approved ICIs that bind PD-L-1 are Atezolizumab for urothelial carcinoma and NSCLC, Avelumab for Merkel-cell carcinoma and Durvalumab for urothelial carcinoma and NSCLC.
To overcome primary or acquired resistance to the existing immune checkpoint therapies, intensive research and development for other immune checkpoint targets are underway. Some of the promising targets under research or clinical evaluation include:
NK-cell reactivation is a newly emerging field, and many NK-cell related immune checkpoints have been identified. Apart from the prominent NK receptors KIRs, LIRs, and NKG2A, NK-cell suppression was seen to be induced via CTLA-4, PD-1, B7-H3, LAG-3, TIGIT & CD96, TIM-3, Siglec-7/9, CD200 and CD47.
Therefore, combination therapies targeting NK-cell specific checkpoints and T-cell/NK-cell checkpoints have been proposed for more potent immunotherapy.
In-vivo studies and clinical trials have demonstrated that dual checkpoint inhibition exhibit a synergistic anti-tumor response over monotherapies. A combination therapy using Ipilimumab (anti-CTLA-4) and Nivolumab (anti-PD-1) significantly improved efficacy in metastatic melanoma patients. Following the trial, Ipilimumab plus Nivolumab therapy was approved to treat metastatic melanoma, advanced renal cell carcinoma and metastatic colorectal cancer with MMR/MSI-H aberrations. Similarly, several trials are ongoing to investigate the efficacy of multiple combinations of immune checkpoint inhibitors and a combination of ICIs with other chemotherapeutic or immunotherapeutic drugs. For example, anti-LAG-3 plus anti-PD-1 and anti-TIGIT plus anti-PD-L1 have shown promising results. Another upcoming strategy that is being explored is the use of bispecific antibody formats to target dual immune checkpoints. For example, AGEN1777 is an Fc-engineered anti-TIGIT bispecific which targets inhibitory receptors T and NK cells to enhance anti-tumor activity.
Evidentic aliquots can be used as positive controls for:
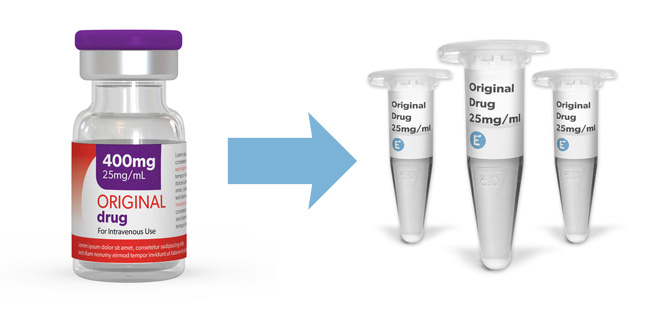
All aliquots contain the clinical-grade molecule of the original drug and are prepared by repacking the content of the original vial into small and convenient aliquots as research consumables.
Clinical-grade molecules as research consumables

Evidentic GmbH
Martin-Buber-Str. 10
14163 Berlin